Downloads
- ashcroft prescribing formulary
- ashcroft repeat prescribing policy
- prescribing rules to aid efficiency in prescribing systems
- downloadable form – patients who want to be able to order via telephone.
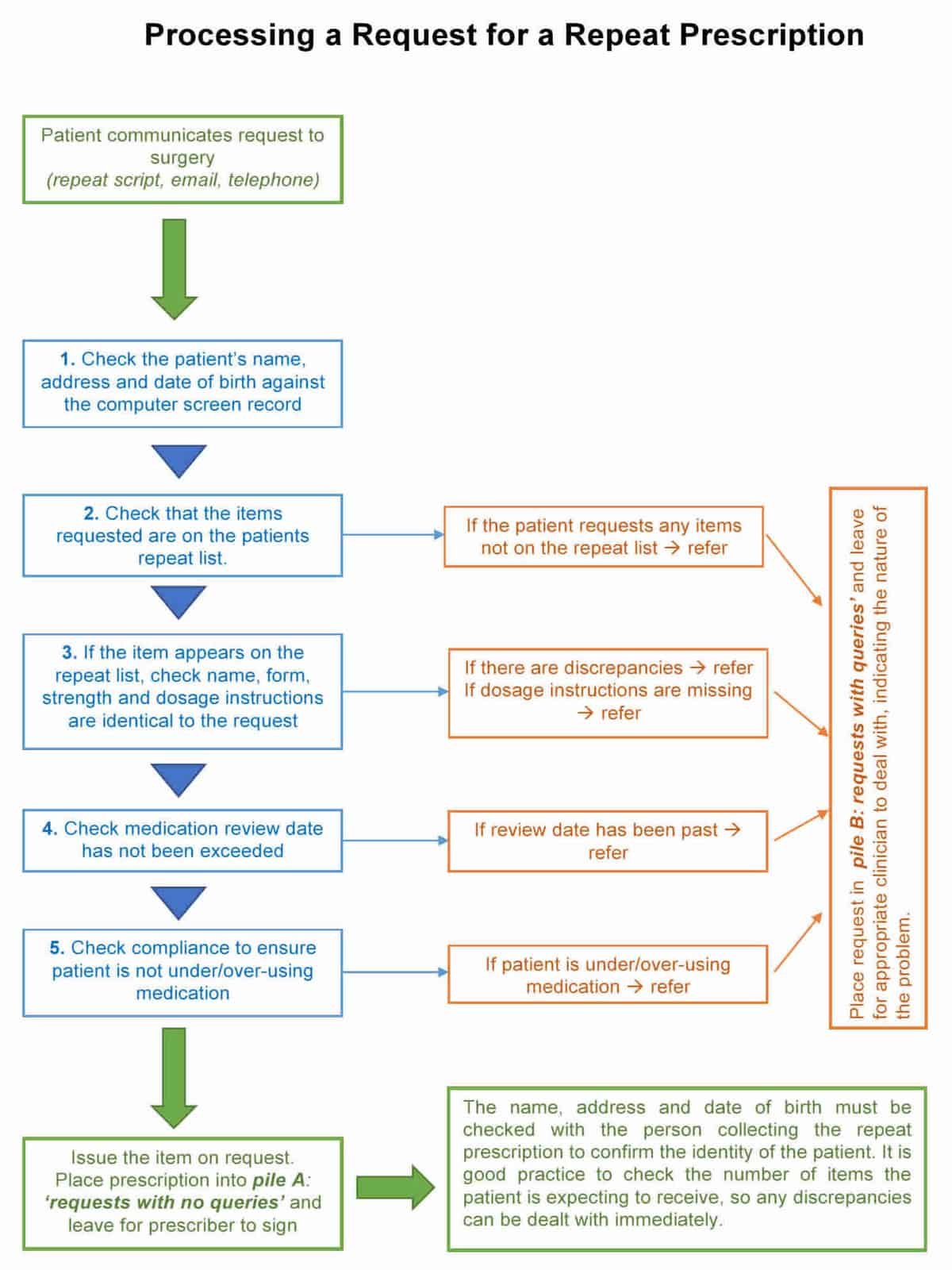
- flowchart: request for a repeat prescription (word doc)
- www.ashcroftsurgery.co.uk/calling-us-about/prescriptions
- NHS Prescription Fraud
ASHCROFT LEADS
- Doctor: Drs. Pardip Sandhu & Jas Dhillon
- Pharmacist: Sadia Khan
- Admin: Carole Middleton
DATE REVIEWED:
20th June 2019
DATE OF NEXT REVIEW:
June 2020
Have you come to the wrong page?
If you are a patient looking for information about how to order a repeat prescription, then you have come to the wrong page. This page is for doctors and staff at Ashcroft Surgery and it outlines the procedure for us to follow when you make a request for repeat medication. Please click the link below which will take you directly to our page for patients on how to order a repeat prescription.
The Policy/Protocol
The aims of this policy
- To standardise repeat prescribing processes
- Understand the acute prescribing process
- To enable staff (admin, doctors, pharmacists and nurses) to understand their roles and responsibilities around acute and repeat prescribing
- To make users aware of a good repeat prescribing process and procedures
- To ensure safeguards are in place to minimise error and reduce risk
Our Prescribing Formulary
This formularly is not exhaustive and not comprehensive. In fact, it’s quite short. The intention is to synchronise what the doctors prescribe at the practice for common conditions based on group discussion of best practice, NICE guidelines and cost vs. benefit. This formulary is reviewed once a year at a PLT meeting which includes our in-house pharmacist.
The Electronic Prescription Service or EPS for short
This surgery processes most of its prescriptions through the Electronic Prescribing System. This is a national system where prescriptions, once electronically authorised and signed by the doctor can be sent electronically to the patient’s nominated pharmacy. Clearly, this is a good thing as it is kind to trees (no more paper) and the transfer of prescriptions is safer and immediate.
Nomination is the process that gives patients the option to choose or nominate a dispensing pharmacy to which their prescriptions can be sent automatically through the Electronic Prescription Service. There is specific legislation which governs nomination for EPS. It states that GPs must not seek to persuade a patient to nominate a specific dispenser; and if asked by the patient to recommend a dispenser to nominate they must provide the patient with a list of all the dispensing contractors in the area who provide an EPS service.
NHS choices (www.nhs.uk) can be used to provide details of which pharmacies are near to the patients home, surgery or place of work. A community pharmacist or a member of the community pharmacy staff must not give, promise, or offer to any person any gift, or reward as an inducement to present an order for drugs or appliances on a non-electronic prescription form, or non-electronic repeatable prescription, or nominate the pharmacist as their dispensing contractor. The CCG will work with key stakeholders such as the LPC and LMC to ensure compliance with legislation.
Prescription Fraud
Prescription fraud can present itself in many ways. The most common scenario of prescription fraud is where a patient has altered a prescription (which they are not allowed to do). Or it might be where it has been collected by an individual pretending to be someone else in order to obtain the prescription. Other examples include: use of computers to create fake prescriptions or impersonating medical staff to pick up a prescription.
But it can also be a someone (like a community pharmacist or surgery staff worker) who signs a prescription who is not authorised to do so! Or perhaps a phamacist who is asking for a prescription to be broken into many parts e.g can you do two lots of prescriptions for drug xxx (so that he or she can claim more money back – which is dependant on the number of items issued).
And finally, let’s not forget healthcare workers are in a unique position to acquire and misuse prescription drugs. Offenders may steal drugs while working, steal prescription pads, or write illegal prescriptions for friends.
- If you suspect prescription fraud, please flag this up to a doctor and the Practice Manager. They will then decide whether it is indeed a case of prescription fraud. If it is, they will inform the CCG’s prescribing lead and consider WYCSA and the police.
- If a pharmacist suspects prescription fraud, take down the details and again notify the Practice Manager and the doctor. Please advise the pharmacist that they should report to the police and WYCSA and that a pharmacist reward scheme is available for doing so.
General FAQs
- If not in holders – look for when patient requested;
- If less than 48 hrs (2 working days), advise patient to call after 2 working days from request date rather than searching further and disturbing the doctors. The doctor may still be processing it. Try not do a duplicate and try not refer onto the emergency doctor (who will already be busy).
- If you do put through any scripts with less than 48 hours notice (e.g. felt critical medication for patient to be without) – must add to the blue board and ask emergency doctor.
- If more than 48 hrs (2 working days) then…
- Check the electronic Prescription Log to see if the patient’s name is recorded and whether the prescription has gone to the chemist. (ring chemist if needs be) – remember, it might have gone electronically – if so, there should be an “electronic stamp”.
- Check GP pigeonholes, their desks and the tops of their printers.
- Chase the doctor who the prescription task was sent to and get them to do it ASAP. Only refer to the emergency doctor as a last resort.
- If the prescription cannot be located – and is not for a controlled/potentially abusive drug – issue a prescription, clearly mark ‘duplicate’ on this prescription and pass onto the on-call doctor. For dangerous drugs like controlled drugs – discuss with GP on-call and see whether they need to see them.
- If you do print off a duplicate prescription – try and nab a GP to sign it when they’re not busy seeing patients. Highlight the fact that the prescription is a duplicate. Als provide a pen for them to sign (the GP may not be carry one on him/her).
- Try to ensure any prescriptions you have promised to provide are signed before you complete your shift or passed onto another member of staff for their overview.
Only qualified prescribers can make clinical decisions and judgement. Qualified prescribers include doctors, some nurses with ‘prescribing rights’ and in-house pharmacists. Under no circumstances should an admin member make a clinical decision about a prescription. Instead, refer to a qualified prescriber. Examples of things which are considered clinical with respect to prescribing are…
- Queries about a medication (for example, if the patient asks about side effects or interactions with other drugs or asking for a medication to come off their repeat list).
- Queries about the dose or a change in formulation (e.g. asking for a liquid rather than a tablet)
- Reviews and Reauthorisation of medication.
- Our Practice Manager will ensure that staff will only have functions on their smart cards which are appropriate to their specific role.
BUT BEFORE YOU ASK A DOCTOR, ASK YOURSELF IF THE IN-HOUSE PHARMACIST/PHARMACY TEAM CAN HELP FIRST.
The practice meets with the our in-house pharmacist at least once per year to review our prescribing behaviour for all of acutes, repeats and medication for chronic disease. It is at this meeting where our Prescribing Formulary is reviewed and necessary changes made in line with good practice.. This annual meeting is completed as part of the practice weekly PLT programme and recorded within the Practice PLT meetings plan
Yes, providing they have consent. The pharmacy must receive written consent from the patient to collect their prescription from the practice using a process which is auditable. This should where possible be from the patient themselves. In certain circumstances it is acceptable for a patient’s representative to provide consent. This may be
- On behalf of a child by their parent or guardian
- On behalf of an adult incapable of nominating a pharmacy by their relative or carer
NB a pharmacy contractor is unable to provide consent on behalf of a patient choosing their pharmacy.
- The patient should receive both written and verbal information explaining the repeat-collection scheme. This should include a statement to ensure the patient understands that they can cancel the collection-delivery arrangements at any point if required. Once the pharmacy has received consent from a patient, it should be clearly marked on the patient medication record within the pharmacy. Where appropriate the pharmacy will also send a copy of the consent to the practice. The chosen pharmacy can be indicated on the patient’s record at the practice and printed on the top corner of the prescription so reception staff can easily identify where the prescription should be sent.
- In cases where a pharmacy receives a prescription not intended for their pharmacy it MUST be returned to the practice.
- If the pharmacy does not have written consent to pick up a patient’s prescription and are requested to do so by the patient they should obtain this as soon as possible e.g. if the patient needs a prescription in an emergency they may telephone the pharmacy to request delivery providing verbal consent which needs to be reinforced in writing.
No. The rules have changed. Pharmacists can no longer do this. This was changed in order to reduce wastage and fraud within the NHS. Some pharmacists would order everything on a repeat list even if the patient did not need them (because it is easier to do this and they get paid for every item). As a result, patients would get upset at the large volumes of unnecessary medication in their homes, which is also wasteful in an NHS where there is limited money. And some medications are VERY expensive (£15-30 per month!).
We would like to make it clear that most pharmacies in the UK do an amazing job, are honest and were not doing this. It was only a few; but it needed stopping.
You have some obligations under your employment contract to provide the practice with data. In particular, you are required to report absences from work and may be required to provide information about disciplinary or other matters under the implied duty of good faith. You may also have to provide the practice with data in order to exercise your statutory rights, such as in relation to statutory leave entitlements. Failing to provide the data may mean that you are unable to exercise your statutory rights.
Certain information, such as contact details, your right to work in the UK and payment details, have to be provided to enable the practice to enter a contract of employment with you. If you do not provide other information, this will hinder the practice’s ability to administer the rights and obligations arising as a result of the employment relationship efficiently.
Employment decisions are not based on automated decision-making.
Requests for ACUTE prescriptions (ADMIN)
An acute prescription is one which has (usually) been given as a one-off and is not intended to be given again and again. For example, a person with ear ache may have been given some ear drops to use for 7 days but that does not mean that patient should get it again and again. And neither should the patient be able to ask for it again if he or she had another episode of ear pain in the future (they should come and see the doctor again). Therefore, patients really shouldn’t be asking for acute medications via the repeat prescribing system – but invariably, they do! In some cases, it is because a doctor has prescribed a drug which should be on repeat but has prescribed it as an acute and only intends to put it onto the repeats once the patient is stabilised on it. In terms of what to say to patients, you might say…
‘Mrs. XXX, did you know that your asking for a repeat of a medication that isn’t on your authorised repeat medication list. Do you know whether the doctor intended to give you this medication as a one-off or whether he plans to keep you on it for a while?’.
And then pass the request onto the doctor.
Patients should not be making request for a repeat of acute prescriptions given in the past. If they do,
- Ask “I’m really sorry, but that prescription is not on your authorised repeat prescription list. Just because it might have been given in the past doesn’t mean you can have it again and again because sometimes, medicines can be dangerous if used in this way. Are you sure it is something you still need?”
- If the reply is yes, then pass this onto the pharmacy team first.
- If they need it ASAP – put it on for the on-call doctor.
- Hospital issued prescriptions should be collected from the hospital pharmacy – not the surgery.
- Advise the patient of this and ask them to go back to the hospital pharmacy to collect it.
- The most common reason why the patient does this is because they refused to wait at the hospital pharmacy. We consider this reason unacceptable as it duplicates unnecessary work for the practice. Please put the onus and responsibility back onto the patient where it ought to lie. If this is not the reason and the reason sounds justifiable, then allow an exception to the rule.
- But remember – the on-call doctor already has enough on his or her plate.
- First of all, tell the Consultant that it is practice policy to ensure authorised prescribers issue their own medication rather than putting the work on overstretched NHS GP practices. So ask them to do it. If their is strong reluctance….
- Ask them if they would mind faxing a request on hospital headed paper to reduce the chances of prescribing errors.
- If they are unwilling or unable to do this, take accurate details of the request – spelling out the name of the drug (do not second guess) and asking for the dosage in both words and numbers (e.g. ‘is that thirty milligrammes as in three zero?’).
- Establish with the Consultant when the patient expects to collect the prescription/medication
- Pass details to GP clearly indicating that this is a Consultant request
If a pharmacist or patient or a relative picks up a prescription – be sure to make a log of it in case we need to do an audit trail if it goes missing. At Ashcroft Surgery, we keep an electronic log.
Our REPEAT prescriptions system
- All prescription requests will be ready within 48 hours (2 working days). The process is outline below. A prescription request will only be delayed if of a complicated nature and the doctor is having to complete additional checks or waiting to then see the patient at an available appointment slot.
- It’s not just the doctor’s responsibility! The production of repeat prescriptions is a team approach with input not only from the doctor or nurse prescriber, but also from other members of the healthcare team to produce high standards of practice and care. If other people don’t do their bit, then mistakes happen in the repeat prescribing process and ultimately, it is the patient that suffers. So, please do your bit.
- Most of the information from these pages is adapted from the document ‘Repeat Prescribing Guidelines’ by Rachel Urban (v.11, Bradford)
A repeat prescription is one which contains medication items which are already on a patient’s repeats medication list section of their medical record. This prescription can be obtained repeatedly when they run out without having to see a doctor. These items should be limited to medicines which are prescribed for long term therapy to patients who are stable. A repeat prescribing system is a system to issue such prescriptions but also includes measures to review the patient and their medication periodically, check concordance, remove any unnecessary medication and make fine adjustments based on good clinical practice.
Repeat prescriptions should be issued to
- patients who have an illness for which long term regular medication is appropriate
- patients who are likely to need a medication repeatedly but not regularly (e.g. gaviscon, lactulose)
Doctors are responsible for initiating repeat prescriptions. The patient must be stable on the medication.
- Authorisation – where the doctor initially puts a medication on repeat
- Medication request– the patient requests he repeat medication via the repeat script (preferred) or electronically. Only in exceptional circumstances will we accept telephone requests.
- Admin check medical records for compliance and review dates
- Admin print the prescription. If all is okay, admin staff print of the prescription and hand over to doctor; if all is NOT okay, admin staff highlight any prescriptions of concern, keep these in a separate pile and then hand these over to the doctor.
- Doctor does a medication review (and read codes it)
- Doctor re-authorises and updates review date (as necessary) on SystmOne.
- Doctor signs the prescription and hands it back to admin staff.
- Prescription storage – admin staff place the prescription in a secure holding area until patient arrives to pick it up.
Authorisation is the decision by the prescriber that a particular medication is okay to have on a repeat prescription for that particular patient. Only prescriptions which have been “authorised” may be issued by non-clinical members of staff. An authorised prescription only includes those medicines on “repeat templates” on SystmOne. It does not include medication that appears in the acute, current of past history sections of the patient medication record. Items on a patient’s repeats should be limited to medicines which are prescribed for long term therapy to patients who are stable. Non-clinical staff can only be allowed to view or issue items already on a repeat list. ONLY members of staff with relevant clinical qualifications are allowed to add medication to records.
Who can authorise medication?
- Doctors, Nurses with a prescribing number, an in-house pharmacist.
To authorise, the doctor, nurse, pharmacist or prescriber must check that
- the patient is stable on the medication,
- the medicine is well tolerated and
- it is still needed.
Medicines that are subject to monitoring and dose titration must not be added to the repeat until
- they are deemed to be safe for that patient
- a stable therapeutic dose has been achieved
- if appropriate – bloods/investigations have been reviewed to check that the drug is okay to give at that dose
- there is a clear protocol for issuing them as repeats.
When prescribing a new repeat, try and syncronise – match up all repeat medications in terms of quantities (that it runs out when other medication runs out) and review dates.
Repeat requests should ideally be received in writing on the repeat slip/ counterfoil, as they are more likely to be processed accurately. In some circumstances it may be impracticable for practices to only receive written requests. In these circumstances admin staff must ensure they ask sufficient questions to process the repeat request accurately (see under telephone header below for more information). Patients should be advised at the time of request that the doctor may wish to see them before the item is issued.
Written Requests
There is evidence to suggest that written requests are more accurate than telephone requests. The patient should tick the items they want on the repeat side of the prescription foil and hand or post it to the surgery. This will be processed within 2 working days. This is the ideal because it (i) minimises transcription errors, (ii) minimises confusion with brand and proprietary name pronunciation, (iii) avoids mismatching the request to the patient’s record, (iv) allows prescriptions to be processed with no interruption from further calls and (v) allows requests to be deposited in a post box in the reception area to avoid disturbing staff unnecessarily. If the patient forgets/ loses the repeat slip then a repeat slip can be printed from the patient’s medication record or alternatively a request slip could be completed by the patient.
Electronic Requests
Staff need to be very careful with requests for repeat medication via e-mail or the internet. Especially check to make sure the item requested matches what is on the patient’s repeat list on SystmOne. Don’t only check the name of the medication, but the strength, the form and the dosage instructions. Also double check name, date of birth, address. And finally, check to ensure that patients are not over or under ordering – SystmOne will tell you. If there is ANY descrepancy, please ring the patient and check it out with them.
Telephone Requests
Remember that telephone requests for medication can (i) block more urgent calls, (ii) block patients trying to make appointments, (iii) distract receptionists whilst processing requests, and (iv) lead to one request not being processed before the next telephone call is answered. Alternatively, if the number of telephone calls are low the receptionist allocated to that role does not have a constant work flow. Where a practice chooses to use telephone requests,
dedicated times should be encouraged to concentrate calls to a specific time releasing the receptionists at other times in the day. This does not mean that patients telephoning outside these hours should be refused medication, instead the request should be accepted and the patient reminded of the designated times when requests should be made.
Compliance – under or over using
- Did you know that you can check compliance through the computer – SystmOne will tell you how often the patient is ordering the medication – and whether they are underusing, overusing or are just right. Repeat prescribing admin staff need to have been trained to look at the compliance section of SystmOne and to tell you if a patient is significantly under or over using a medication. whether the patient is taking the medication as prescribed (i.e. is concordant) and not underusing or abusing it. Check under ‘history’ in SystmOne to ensure the patient is not ‘under using’ for ‘over using’ the drug.
- The Practice Manager will check that the computer is set so that compliance issues are flagged and a message over ridden before the receptionist can continue. There is evidence to suggest that on screen reminders are more effective than feedback in modifying behaviour related to medicines management.
- Early requests for items can be permitted in certain circumstances i.e. if a patient is due to go on holiday, even though the computer will identify this as overuse.
- Medicines which can be taken on a ‘when required’ basis may be flagged by the computer as being underused e.g. pain-relief, indigestion remedies etc. Staff who process repeat prescriptions should be aware that this is acceptable although should still be brought to the doctors attention. The practice should develop their own list of medicines which they feel are acceptable to be under-used.
Review Period
- Check that the repeat item is within the authorised period – i.e. the review date has not been exceeded OR the number of authorised prescriptions has not been exceeded. If it has, then do NOT issue the prescription and refer the case to the doctor or prescriber.
- If the review date is approaching, the item can be issued and the patient informed that a review appointment is due e.g. highlighter or stapled note attached to the prescription. Where prescriptions go direct to the pharmacy, the pharmacy staff should indicate to the patient that a review appointment needs to be made.
- Repeat prescriptions need to be prepared with accuracy by a receptionist who is trained up in the role of repeat prescribing.
- In order to reduce the risk of mistakes, the receptionist who has the task of processing the repeat prescriptions should do so in a quiet area where they can concentrate and not be distracted.
- A computer system must be used to issue all prescriptions.
- Before you issue the prescription
- Check SystmOne to see if the patient is underusing or overusing the medication significantly. You should know how to do this, if not, ask a colleague. If they are under or overusing, please write this on the right hand side of the printed prescription and highlight it with a highlight marker for the doctor to see. Early requests for items can be permitted in certain circumstances i.e. if a patient is due to go on holiday, even though the computer will identify this as overuse. Medicines which can be taken on a ‘when required’ basis may be flagged by the computer as being underused e.g. pain-relief, indigestion remedies etc. Staff who process repeat prescriptions should be aware that this is acceptable although should still be brought to the doctors attention. The practice should develop their own list of medicines which they feel are acceptable to be under-used.
- Check that the repeat item is within the authorised period – i.e. the review date has not been exceeded OR the number of authorised prescriptions has not been exceeded. If it has, then do NOT issue the prescription and refer the case to the doctor or prescriber.
- If the review date is approaching, the item can be issued and the patient informed that a review appointment is due e.g. highlighter or stapled note attached to the prescription. Where prescriptions go direct to the pharmacy, the pharmacy staff should indicate to the patient that a review appointment needs to be made.
- Prescriptions need to be printed and processed within 48 hours of recieving the request from the patient. When accepting a request from a patient for a repeat prescription, please tell them that the turnaround time for a prescription will be 2 days and that they should not come to collect it before then.
It is important to ensure prescriptions are issued via SystmOne rather than hand-written because computers…
- Warn of possible interactions, contra-indications and side effects.
- Provide a record of the issue in the patients notes – so that others can see what has been given.
- Provide the patient with a copy of the items that have been authorised as a repeat prescription, which can be used to request a repeat.
- Can be used as a source of data and audit to improve prescribing quality and maximise cost effectiveness.
- Provide the doctor with a profile of their prescribing habits.
During a review patients should be considered individually, with respect to their illness and medication. The person reviewing the patient should be satisfied that the patient still requires long term medication and will check the items listed below. All queries and complex issues should be referred by the nurse to the doctor. If a patient fails to attend for their Medication Review repeatedly, consider doing it opportunistically when they present acutely. A medication review can be done by a doctor, an inhouse pharmacist or an appropriately qualified nurse (with prescriber status). Not all medication reviews need to be done face-to-face either. Many can be done over the phone – especially where the patient is on four or less medication repeats. Medication Review and Re-authorisation of medication should be done at the same time.
For each individual medicine…
- Does the patient understands the purpose of the medication
- Are the dosage instructions are clearly written on the prescription. If the prescription states ‘when required’ then a maximum dose needs to be stated. MDU or ‘as directed’ are not acceptable.
- Is the patient taking the medication as prescribed (i.e. is concordant) and not underusing or abusing it. Check under ‘history’ in SystmOne to ensure the patient is not ‘under using’ for ‘over using’ the drug.
- Does the drug continue to be effective – is it having the desired effect, are they on the right dose? Is there a better and more suitable alternative?
- If the medication is no longer necessary remove it.
- Is the patient is experiencing any intolerable side effects? (Side-effects/ ADRs/ allergies should be recorded in the patient’s notes.)
- Change the medication to generic form if appropriate (exceptions listed below). If you do this, inform the patient that you have changed the name of his/her medication, but that it is chemically the same. Alert the patient to any change in appearance of the drug. (Nurses – If in any doubt, consult the doctor)
- Review any bloods (e.g. TFTs for thyroxine, TFTs and Li levels for Lithium, CVD bloods, Renal Bloods, Rheumatology bloods and so on)
- Have appropriate measurements and examination been done? – eg BP, HR, ECG
- Reauthorise to allow 12 months (6 months in over 75’s) of repeat medications.
- Code Medication Review Done on the computer (this is part of the template).
- Document any changes in the patient’s notes. Any change should be monitored, and be reviewed again at reauthorisation or when medication review is due in line with QoF.
For the repeat prescrbing list as a whole…
- Determining which medicines are being taken and deleting any medicines which are not being ordered and duplicate medicines. It is good practice to periodically run searches to determine which medications are not being ordered.
- that all medication is prescribed in equivalent quantities (so, for instance, they all run out at the same time, enabling the patient to re-order everything in one go where possible). The quantities must be sufficient and not excessive.
- that prescribing is generic where appropriate
- other medications prescribed from other organisations and over the counter medicines are identified and listed.
- that the patient has been informed of the next review date
Other considerations for the doctor’s medication review
- Check that each prescription has a relevant ‘indication’ item on the computer.
- Check that the prescription is appropriate within the prescribing incentive scheme markers
- Stop any medications that are not being ordered regularly
- Consider dossett boxes in elderly patients or those on complex polypharmacy
- Consider referral to case manager in patients with complex polypharmacy (more than 8 medications on repeat)
- Consider review by pharmacist in complex polypharmacy
Drugs that should NOT be prescribed generically…
- Diltiazem
- Nifedipine
- Isosorbide mononitrate
- Theophylline slow release preparations
- Anticonvulsants
- Mesalazine
- Insulin
Reauthorisation
All repeat medications must be commenced on the computerised patient repeats prescription list by a GP and authorised for a set number of issues. Once this number has been achieved it has to be re-authorised by the GP. The GP should try to synchronise the list of repeat medications to need re-authorising at the same time and at this re-authorisation carry out a formal medication review. It’s also good practice (and it saves a lot of work) if one can do medication reviews and reauthorisations at opportunistic times like at the chronic disease review clinics. If you are doing a reauthorisation, also try and do a medication review.
Remember: reviews don’t necessarily have to be done face-to-face. There is the option of the telephone! Give message to the reception staff to ask patient to make appointment for Medication Review. If any blood tests are required give clear message to the receptionist to book these prior to the review and note in consultation record which bloods are required. The medication review can still be booked as a telephone consultation if appropriate.
The Review Date
- Normally the review date for stable medicines is set at 12 months but it should be set earlier for patients who should be seen more often (e.g. older people on polypharmacy set for 6 months).
- Review dates are the key to managing long term medicines.
- The review date acts as a safety mechanism to ensure that medicines are flagged back to the prescriber for review.
- When you are asked to review a medication, try and review ALL the medication on repeats and set the review date for ALL those medication. Read code that a medication review has been done (their is a tick box for this in SystmOne when you reauthorise medication – left hand side at the top of the page).
- It is preferable to have a review date rather than a maximum number of issues.
- The review date should be the same for all the medicines (except those where a particular medicine may need an earlier review). This ensures the patient’s medicines are reviewed holistically.
- Only a clinician or an in-house pharmacist should update the review date.
- The review date must be updated each time a medicine is added or changed.
- An entry needs to be made in the medical records at the time of medication review to indicate that it has occurred, noting any changes.
- The prescriber should have access to the patients’ medical notes when signing/ re-authorising repeat prescriptions.
- Once prescriptions are signed, they should be stored in a secure area away from public access. In Ashcroft Surgery, there is a prescription filing cabinet in the receptionists area (which is partitioned off from the patient waiting area).
Requests for REPEAT prescriptions (ADMIN)
All scripts requiring a doctor’s agreement and signing will be sent to the Electronic Prescribing System intray. That is where you will send the requests.
- There is a doctor nominated each morning and afternoon (maked with a YELLOW appointment slot in their surgery) who will be responsible for dealing with these scripts.
- Please send them a screen message midway through their surgery to do those scripts. “Please don’t forget to do the EPS when you have time.”
- At the end, check the EPS is near empty. If not, contact the doctor again.
- Only pass on urgent requests to the on-call doctor.
- Any prescription queries should go to the in-house pharmacist/pharmacy team.
There may be three situations for this…
- The drug is on the repeat list but under a different name.
- All drugs have two types of names – one is called the generic name (e.g. Ranitidine) and the other is called the trade name (e.g. Zantac). The generic name is usually the ‘medical’ name by which that medication is known throughout the whole world. However, trade names can vary from country to country and is often given by the company that makes that drug. A single drug can be made by many different companies throughout the world. In this example, the patient might ask for Zantac, but on their repeat prescription, it will be listed as Ranitidine.
- So – look at the BNF or MIMS to see what alternative names their are for a drug. Once you’ve found it, ask the patient to always try and ask for that drug under that name.
- The drug is not on their repeat list – but it is on their acute list.
- Look at both the repeat list and acute list of medication given in the past.
- Tell the patient that you cannot see it on their usual set of repeat medicines and ask them politely why they are making the request.
- Advise them that you can see it on their acute list but ask them whether they know if the doctor planned to give it as a one-off or as something to be taken regularly.
- If the patient says it was a one-off, advise the patient they shouldn’t be asking for it again and again. Ask if they wish to talk to the doctor.
- If the patient says it was meant to be a repeat, pass onto the doctor with a note asking if it should be on a repeat.
- The drug is not on their repeat list nor under their acutes.
- Tell the patient that you cannot see it on their usual set of repeat medicines and ask them politely why they are making the request.
- Check patient letters – to see if request is from hospital consultant/Clinic
- Tell them that drugs not given by the doctor cannot be given without the doctor assessing them first.
- Patient should see or talk with a GP for a decision on whether to give the medication or not.
Normally the practice does not allow ordering of repeat prescriptions over the telephone. Patients need to order using their green repeat prescription slips which can be posted or hand delivered – there’s an internal prescription box for in hours and a letter box for out-of-hours. Alternatively, they can email an instruction. Telephone ordering is not allowed for two reasons:
- to ensure the telephone lines are open for appointments use and
- lesson risk of mistakes as a result of mishearing something.
If the patient has not been approved for telephone ordering of repeats
However, if a patient or (on their behalf) a relative, friend or carer, feels it cannot be posted, hand delivered or e-mailed then the patient can request (by filling in a practice form) for practice doctor approval to telephone repeat script requests. You can download this form here: Downloadable Form – patients who want to be able to order via telephone. Please advise the patient that this is only allowed in exceptional circumstances – for example, a bed-bound patient who has no carers or relatives nearby. If the clinical circumstances lead to practice doctor’s approval then:
- Put a code on the patient’s notes in Active Problems page list e.g. ‘telephone prescriptions allowed’
- Acute medication will still require a doctor consultation.
- Returned request forms should be given to the Practice Manager who will confirm the authorisation in writing to the patient.
If the patient has been approved for telephone ordering of repeats
Patients should only be ringing for repeat prescriptions during 2-4pm on Tuesdays, Wednesdays and Fridays. If they ring outside these periods, deal with their query as a one-off and advise them of the correct times.
- Confirm that the patient is authorised by looking for code & description in Active Problems list.
- Remember, that the request should only be for repeat prescriptions. They need to consult a GP if the item is not on the repeat list.
- Confirm to which chemist – if they want to collect it or get it collected by a friend or relative, then politely ask them why this not done to deliver the repeat slip.
- Print script(s) and put for Doctor to sign as per part a) of this protocol.
- Don’t forget to ask for the basics….
- Patient’s Full Name
- Date of Birth
- Address
- Telephone Number (on which to be contacted should the prescriber refuse to issue the request).
- Then question the patient carefully to ensure that
- their medication has not changed since their last repeat e.g. Have you visited the doctor since your last repeat prescription? Have you started any new medication/ changed any of your medication?
- only the medication required is ordered. The patient should be asked about each item individually rather than asking whether they would like all items on their repeat.
- For each item, ask about
- Name of drug
- Strength
- Form
- Dosage Instructions
And finally, remember that some of these patients might benefit from email us their required repeats rather than telling us over the phone – so advise them as appropriate to their abilities and resources.
- Explain politely (again) why we don’t take requests over the telephone because of the likelihood of hearing mistakes and because we need to keep phone lines open for patients trying to get to see the doctor – i.e. appointments.
- If the prescription is not needed urgently, ask them to present their completed request form.
- Suggest other ways to request scripts (email, fax, friend/neighbour/relative to help).
- Do issue this time, but explain that this is a one-off favour to them and update the screen message (i.e. told twice not to ring) & date this.
- If you feel the patient would struggle with posting, delivering, faxing or emailing, then advise them of the possibility of ordering over the phone – but that they need to fill our a telephone request for medication form first using this form: Downloadable Form – patients who want to be able to order via telephone.
Prescriptions need to be printed and processed within 48 hours of recieving the request from the patient. When accepting a request from a patient for a repeat prescription, please tell them that the turnaround time for a prescription will be 2 days and that they should not come to collect it before then. However, some patients leave it until the very last minute and order their repeats when they are running extremely low and end up needing the repeat script urgently. In such cases, please issue the script and get it signed in a timely manner (less than 48h) but then tell the patient about this extra duty and what they might do in the future to make life more smoother.
For instance, you might say ‘Mrs. Brown, you’re prescription is now ready for you to collect. Normally we ask all our patients to give us a minimum of 2 days to process the prescription but for you we did it sooner because we know how desperately low you’ve got with your medication. Can we politely ask in the future that you try and order your repeats about a week before you are due to run out. In that way, it gives both of us time and makes both our lives easier. Otherwise it creates a bit of havoc. Is that okay’
- Ask the patient why they feel it is urgent. If you feel it is urgent (e.g. asthma inhalers, heart medication) issue the prescription and pass onto the on-call doctor. Explain politely (especially to patients who left things till the last minute) why we say a prescription will take 48 hours; in particular…
- That Ashcroft Surgery is a very busy surgery
- Therefore, we need time to process the request
- And that urgent requests like these result in interrupting the doctors who are already busy seeing ill patients.
- And that urgent requests like these create unnecessary chaos for the practice who already have much to do.
- Give the patient a time to return to the Surgery to collect the prescription later that day. DO NOT MAKE THIS TIME TOO TIGHT! Otherwise you’re only setting up the practice for failure and the patient will be really upset when they come in and the prescription you said would be ready is not ready! And then they’ll take it out on you.
- Try to ensure that any prescription you have ‘promised’ is signed & available for collection before the end of your shift or agree with another member of staff for them to oversee it.
- If a patient is in surgery and being insistent they want it ‘now’ – give them the option of waiting but also tell them that there may be a lengthy wait. Explain to them that their immediate request puts unnecessary pressure on the practice because it interrupts GPs who are busy attending to patients. Explain that on this one occasion we will do them a favour but it still will involve a significant wait.
e.g. asks for a TWO month supply of something or asks for TWO x inhalers rather than their usual amount of ONE.
- Contact patient to find out why – ask the patient politely.
- If the reason is valid (e.g. a holiday) issue but indicate on the prescription that this is an additional request and state the reason to help the GP to decide.
- Put a clear message on the computer record: that additional medication has been issued & why or if refused, why the GP has done so.
- If the request is reasonable – issue additional items and make clear note on computer screen
- Attach note to prescription(s) detailing reason for additional medication for GP approval and signature
- Issue but post-date prescription if holiday is in this country
- Admin highlights the review due on the prescription before passing it to a doctor to sign.
- Doctor to check review date is accurate – for example, has a review been done but date not reset?
- Doctor does review if possible from clinical record and sets new date. Do a review of all the medication on repeats at the same time. If it is too complicated to do through looking at their records alone, ask the patient to come in for review with a doctor (preferably the doctor asking for the review).
- If 3 months have lapsed after the review due date, the Doctor either
- refuses to issue until review completed (depends on clinical risk of not having medication) or
- issues for 7 days to provide time for review to occur; the patient must be informed that no further medication will be given after this prescription and must attend the review appointment.
- Try to find out why the patient is asking for more medication before the expected time – ask the patient.
- Print the prescription and mark clearly – ‘Over-using’ for GP to make decision
- If ordering very early (and no explanation is available) do not issue but put clear message on screen. Again, contact the patients as to why they are asking for it so early.
This may mean that the patient is not using their medication in a way that is prescribed by the GP. In fact, it could even mean that they’re not using it at all. But also, the computer might be wrong; for instance, they may be getting the prescription from hospital. So…
- Ring the patient to find out what the real reason is behind the under usage.
- Then issue the prescription but bring it to the attention of the GP with a note on the prescription saying ‘Under-using’ and give the reason for the underusage if you have managed to determine it through talking with the patient.
- If it is a replacement request, the patient needs to contact the Air Products oxygen cylinder provider direct with whom that should have been authorised with via the HOOF process.
- New requests (or amendments to existing requests) need to go to the doctor – who will then decide whether indicated and if agrees, to fill new consent & order forms and send to supplier (via the HOOF form – which is on SystmOne).
- Stoma appliances – i.e. leg bags/night bags etc. must be on a separate prescription (even if other medication is being ordered at the same time).
- Check that the serial numbers of the appliances correspond with the request.
- Please make sure the numbers are on the request form because stoma appliance prescriptions can be very complex and hard to find on SystmOne without the numbers.
- These should NOT be shared out but instead be handed over to the doctor with the lead responsibility for that nursing home. That doctor will be familiar with these (often) more complex patients and whether there is unnecessary polypharmacy and whether the home is falling into bad prescription request habits.
- A pharmacy should not be ordering repeat medications on behalf of a nursing or care home. The nursing or care home needs to assign a delegated member of staff to do this task themselves as they are in a better position to ascertain exactly what they do have and what they don’t.
- The following doctors look after the following nursing homes…
- Ashcroft Nursing Home – Dr Liz Hamblin
- The Mount Nursing House
- Idle
- Pollard House
FAQs for DOCTORS
- Prescription quantities should be in multiples of 28 usually not exceeding 90 days.
- For certain medications (HRT, contraceptive pill) you can give more e.g. 6-12 months worth, providing patients are stable and on stable therapy regimes. The first prescipriton for HRT and COC (i.e. when initiating) should be for 3 months and then 6 monthly after that if stable and even up to 12 monthly if stable after that.
- Consider the needs of certain patients e.g. who work away for 3 months, and therefore need a 3 months supply each time.
- It is preferable to issue whole pack sizes (sometimes 30) rather than 28 days as this avoids wastage and broken packs.
Prescribing medicines generically rather than by brand name can improve cost-effectiveness and is encouraged. However, there are some circumstances in which brand-name prescribing is preferred. These include:
- Where there are important differences in formulation between brands of the same medicine.
- Where products contain multiple ingredients and brand name prescribing aids identification.
- Where modified release preparations are not interchangeable.
- Where administration devices (e.g. inhaler or self-injection) have different instructions for use and patient familiarity with the same product is important.
- Where different preparations of the same medicine have different licensed indications.
- Where there is a difference in bioavailability between brands of the same medicine, particularly if the medicine has a narrow therapeutic index.
- Where the product is a biological rather than chemical entity.
This list is not exhaustive and inclusion in this table does not imply endorsement of use.
| Medicine Category | Genericname / group | Comments |
| Drugs with a narrow therapeutic index. | Aminophylline | Difference in bio-availability may affect plasma concentrations. |
| Ciclosporin | ||
| Carbamazepine | ||
| Lamotrigine | ||
| Lithium | ||
| Phenytoin | ||
| Sodium valproate | ||
| Tacrolimus | ||
| Theophylline | ||
| Certainmodified-release preparations | Diltiazem | Different formulations of these modified-release (m/r) preparations may have different clinical effects. |
| Mesalazine | ||
| Nifedipine | ||
| Controlled Drugs including patches(Schedule 2 and3) | Morphine | Caution – differing dosage regimes for SR and XL preparations. |
| Oxycodone | ||
| Fentanyl | ||
| Buprenorphine | ||
| Inhalers | CFC Free Beclometasone | Always state the type of device e.g.accuhaler, turbohaler. |
| Dry powder devices | ||
| Multi-ingredient products | HRT | Generic prescribing may not be practical or may cause confusion due to multiple ingredients. |
| Oral contraceptives | ||
| Antacid preparations | ||
| Multi-ingredient ENT preparations | ||
| Multi-ingredient laxatives | ||
| Bath oils, creams, liquids or gels | ||
| Antiseptics | ||
| Disinfectants | ||
| Miscellaneous | Antipsychotic depot injections | These should be prescribed using the brand name to avoid confusion. Generic prescribing for these drugs may affect clinical response or contribute to dispensing or administration incidents. |
| Stoma care products & appliances | ||
| Wound products | ||
| Insulin | ||
| Nutritional products | ||
| Vaccines | ||
| Nicotine Replacement Therapy |
- Diltiazem
- Nifedipine
- Isosorbide mononitrate
- Theophylline slow release preparations
- Anticonvulsants
- Mesalazine
- Insulin
If a drug is ordered repeatedly on acute basis and the doctor is satisfied that the prescription is appropriate and necessary, then it is permissible to put the prescription on a repeat. But before doing this, think about the implications of doing this carefully. For example, does the patient really need this medication? Are we over-medicalising the problem? Are we creating medication-dependency? Is putting the medication on repeat actually sorting the problem? Have we looked at the problem in enough detail?
If a receptionist tasks you with a medication request where the patient is asking for an acute prescription again – if you are not happy to put them on repeat, think about bringing them in for a review and discussion. Give the receptionist this message in clear terms.
The practice and prescribers should create a guideline about which medicines they are happy to issue on a repeat basis and which ones they are not.
Drugs that you should seriously think twice about before putting on a repeat
- Antibiotics, antivirals and antifungals
- Night sedatives like Temazepam, Zopiclone and so on. These are addictive.
- COC pill and HRT – if patients are stable on these and their BP is okay, we issue 12 months at a time. We don’t put the medication on repeat as a way to ensure that they come in for their review.
- Potentially addictive medications like DF118, Tramadol etc.
- Nutritional supplements (unless clear advice from dietician) – they are expensive and have a black market value!
- Baby milk unless clear clinical indication
- There may be a justification if there is a long term need e.g cystiuc fibrosis, recurrent UTI etc.
The following drugs are okay for repeat
- Antidepressants
- Antipsychotic Drugs
- Anti-mania medication
- Hypnotics
- Benzodiazepines
- Anxiolytics
- Controlled drugs (Schedule 2 or 3)
But the important thing is to ensure there is a REVIEW in place.
There are some patients for whom it is dangerous to have monthly repeat medications. Here’s a list of them and it should be pretty self-explanatory as to why.
- Suicidal patients
- Patient who you suspect will abuse medication
- Terminally ill palliative care patients – whose medication will need altering on a week by week basis, if not more frequently.
If patients has failed to attend for review after 2 requests consider withholding prescription until seen. If a patient fails to attend for their Medication Review repeatedly, consider doing it opportunistically when they present acutely. Also consider ringing rather than writing to them (admin staff can do this).
Hospital letters and discharge medication must be reviewed by an appropriate clinical member of staff for newly initiated medicines and alterations to previous therapy, and the repeat system updated. At our surgery, it is mostly done by the in-house pharmacy team.
- Hospital formularies are often very different from a general practice formulary. Whilst in hospital, medicines may be temporarily substituted and not changed back once the patient is discharged – look out for any changes and remember to make the switch back.. Also remember that a medicine initiated in hospital may have a cheaper alternative in the community which is equally effective.
- Evidence should be sought that:
- The medicine is intended to be repeated
- There is no unintentional duplication of existing medication
- Medication has not been stopped by the hospital in error.
- It is important to establish who is to undertake long-term prescribing and who is to review progress. Some medicines for example might be subject for review at the post discharge outpatient clinic whilst the hospital explicitly ask the GP, or more often, implicitly expect the GP to make dose titrations and perform monitoring. There needs to be a clear protocol for issuing repeat medication subject to the results of clinical investigation e.g. blood monitoring reports and their interpretation.
- Yes, absolutely. How else will you know whether you future prescribing interactions with these drugs? Can you see how dangerous it can be if you don’t?
- But there is a way to do it specifically on Systm1 – where you can add a medication to the repeat list and tag that it is supplied by another organisation (e.g. in this case, the hospital), so that we don’t end up issuing it and prevents over-ordering.
- Examples of medicines supplied by hospital include warfarin, anti-TB drugs, and transplant medicines.
- For medicines of a more specialist nature, shared care arrangements must be provided by the specialists before the GP can prescribe e.g. DMARDs, transplant drugs.
- The shared care protocol defines who takes responsibility for diagnosis, monitoring and prescribing and under what circumstances responsibility for prescribing should be handed back to the specialist.
- Make sure there is an agreed shared care protocol outlining these things before you agree to taking on the prescribing of a drug that you are unfamiliar with.
- So called “red drugs” or hospital only are drugs that should not be prescribed in primary care. These include items such as chemotherapy and drugs being used out of license e.g. sildenafil for Crest syndrome or primary pulmonary hypertension.
- Remember: by signing the prescription the prescriber assumes legal responsibility therefore the prescriber must be satisfied that he/she has the necessary clinical knowledge and skills before taking on the prescribing of any medicine.
“Specials” is a term applied to a group of medicines that do not have product licenses. They are usually very expensive and require the community pharmacist to order the product in specially. They are often listed on the practice medical computer system but characteristically they have no price listed against them.
“Non Multilex drugs” are drugs not on the GP computer system’s pick list of medicines. Prescribers can create non-multilex additions to the prescribing system but this would be in exceptional circumstances. If it does not appear on the list there is probably a good reason. In this situation seek advice from clinical pharmacy support.
There are five main reasons why GPs should not prescribe a special without being fully aware and having considered alternatives.
- The product may not have a product license and therefore the prescriber is liable for the product quality.
- The medicine is often very expensive e.g. calcium carbonate liquid special 120mg/5ml can cost £1,236 per item. Yes, it is that shocking!
- The supply is not guaranteed and the patient may have periods without treatment.
- It causes significant inconvenience for the community pharmacist to obtain the supply.
- Some specials are not listed on GP systems and have to be entered as non-multilex drugs. Consequently drug interactions/cautions etc are not highlighted e.g. methotrexate special and penicillin. In other words, it can result in dangerous medical prescribing errors in the future.
So, before prescribing a special ask the following questions.
- Is there a valid indication? There may have once been a valid indication but the patient may no longer be likely to be benefit
- Is the medicine reasonable to be prescribed by a non-specialist? The medicine may be appropriate for the patient but of a specialist nature.
- Can the patient really not swallow solid dosage forms?
- Is there a licensed equivalent? Use the BNF or the Drug Tariff to identify if there is another product that you can use as an alternative.
- Is there a less expensive special? If a liquid must be used and there is no licensed alternative then consider a special that is less expensive. Ask clinical pharmacy support for advice.
- Be careful with prescribing liquid medication – some are specials and very expensive.
Liquid medications are often incredibly expensive compared to tablet/pill versions. Therefore, exercise caution when nursing or care homes ask you to switch a patient’s medication to liquids because of alleged ‘swallowing difficulty’. Can the patient really not swallow solid dosage forms? Follow the general rule of thumb that if the patient can eat food, they can swallow pills and tablets. And remember, many tablets can be crushed (ask the nursing home to liaise with the pharmacist).
Batch Dispensing allows pharmacies to manage and dispense repeatable NHS prescriptions in instalments for medicines and appliances, in partnership with the patient and the prescriber. The pharmacist ascertains the patient’s need for a repeat supply and communicates any clinically significant issues to the prescriber. The aim of the service is to increase patient choice and convenience, to minimise wastage, to reduce the workload of General Medical Practices and to enable pharmacies to manage their workload.
The patient is given a repeatable prescription plus a number of batch issues (up to 12) which are usually held in the pharmacy (see NHS Bradford and Airedale Repeat Dispensing Manual for further details). Once the Electronic Prescription Service is established the batch issues will be stored electronically on the NHS spine and accessed up to 7 days before a repeat is required.

Are you American by any chance? We spell it as authorisation in the United Kingdom.